Introduction: The Engine of a Thriving Healthcare Business

Running a successful healthcare practice today means much more than just providing excellent clinical care. We are also managing a complex business. This involves countless daily tasks, from handling finances to ensuring every patient feels valued. Medical Practice Management is the essential framework that brings all these pieces together.
So, what exactly does medical practice management involve? It’s the strategic oversight of all administrative and business operations within a healthcare setting. Our aim is clear: to boost efficiency, strengthen financial health, and consistently deliver outstanding patient experiences. You can find a detailed definition of this critical field here.
Why It’s More Critical Than Ever
The need for effective practice management has never been greater. We face rising operational costs and changing patient expectations. Navigating complex regulations, preventing staff burnout, and staying competitive are constant challenges. Patients are also more informed, with 83% researching health queries online. To succeed, we must optimize every part of our practice. This includes smart sourcing of supplies and exploring new specialized services, such as innovative approaches like peptide weight loss treatments, to meet diverse patient needs.
In this extensive guide, we will explore the core components of effective medical practice management. We will look at how to master financial health through Revenue Cycle Management (RCM), improve operational efficiency with technology, and strategically source supplies and specialized services. Our goal is to help you drive growth and lift the patient experience, ensuring your practice thrives in today’s dynamic healthcare landscape.
Mastering Financial Health Through Revenue Cycle Management (RCM)
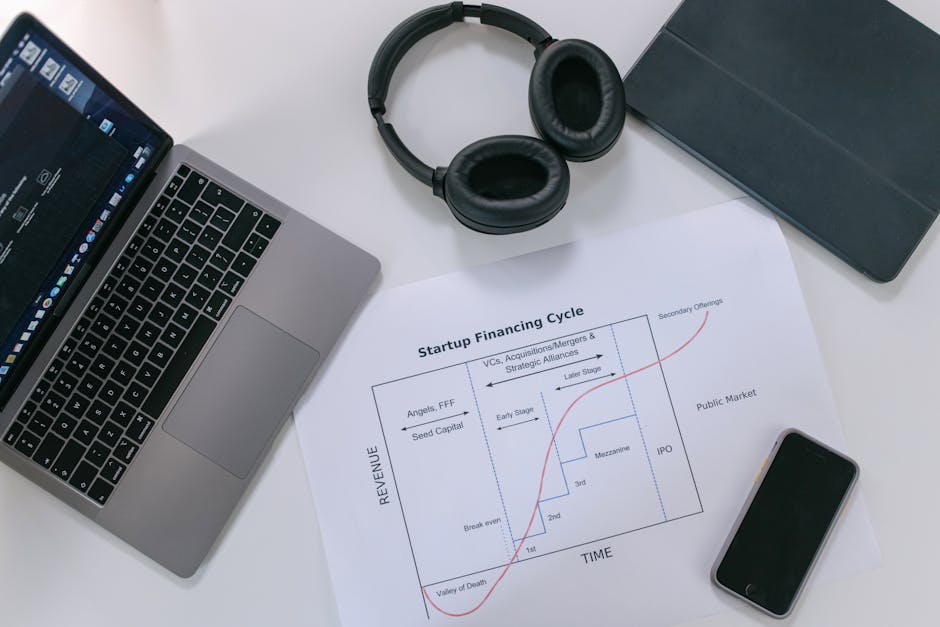
At the heart of any thriving medical practice lies robust financial management. This is where Revenue Cycle Management (RCM) plays an indispensable role, orchestrating the entire financial journey of a patient from their first contact to the final payment. Understanding and optimizing RCM is not just about getting paid; it’s about ensuring the long-term sustainability and growth of our practice.
The Core of RCM in Medical Practice
Revenue Cycle Management encompasses all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue. It’s a continuous process that begins the moment a patient schedules an appointment and concludes when all payments for services rendered have been collected. The global revenue cycle management market was estimated at a staggering $344 billion in 2024, underscoring its immense importance in the healthcare ecosystem. For a comprehensive overview of this critical process, you can refer to the Wikipedia article on Revenue Cycle Management.
The typical stages of RCM include:
- Patient Registration: Accurate collection of demographic and insurance information is the first, crucial step. Errors here can cascade through the entire cycle.
- Insurance Verification: Confirming patient eligibility and benefits before service delivery helps prevent denials and clarifies patient financial responsibility.
- Charge Capture: Ensuring all services provided are accurately documented and billed. This includes CPT and ICD-10 coding.
- Claims Submission: Electronically submitting clean claims to payers, free of errors, to expedite reimbursement.
- Denial Management: Proactively identifying, analyzing, and appealing denied claims to recover lost revenue.
- Payment Posting: Accurately applying payments received from payers and patients to their respective accounts.
- Patient Billing: Generating clear and timely statements for patient balances after insurance processing.
Effective RCM minimizes billing errors, maximizes reimbursements, and ensures a steady cash flow, which is vital for covering operational costs and investing in practice improvements.
Technology’s Role in Financial Optimization
Modern medical practices rely heavily on technology to streamline RCM. Practice Management Software (PMS) is central to this, automating many of the manual tasks traditionally associated with billing and collections.
- Automated Billing: PMS facilitates the rapid and accurate generation of claims, reducing human error and accelerating submission.
- Claims Scrubbing: Before submission, PMS can “scrub” claims for common errors, ensuring they meet payer requirements and significantly reducing denial rates.
- Electronic Remittance Advice (ERA): PMS can automatically process ERAs, matching payments to claims and posting them to patient accounts, saving countless hours of manual data entry.
- Key Performance Indicators (KPIs) and Financial Reporting: Robust PMS solutions offer dashboards and reports that provide real-time insights into the practice’s financial health. These dashboards track critical KPIs such as days in accounts receivable, denial rates, collection rates, and payer mix. This data empowers practice managers to make informed decisions, identify bottlenecks, and optimize financial strategies. For a deeper dive into how analytics can improve practice performance, explore resources like this guide on practice management analytics.
By leveraging these technological tools, practices can transform their RCM process from a reactive, error-prone system into a proactive, efficient, and financially optimized engine.
Ensuring Compliance and Security
The financial aspect of medical practice management is inextricably linked with regulatory compliance and data security. Healthcare is one of the most heavily regulated industries, and adherence to these regulations is non-negotiable.
- HIPAA Regulations: The Health Insurance Portability and Accountability Act (HIPAA) mandates strict rules for protecting patient health information (PHI). All RCM processes, from data entry to claims submission and payment processing, must be HIPAA-compliant to avoid severe penalties.
- Medical Coding Rules: Accurate medical coding (using systems like ICD-10 for diagnoses and CPT for procedures) is fundamental to proper billing and reimbursement. Incorrect coding can lead to denied claims, audits, and potential fraud investigations. Staying updated on the latest coding guidelines is crucial. Resources from regulatory bodies like the Centers for Medicare & Medicaid Services (CMS) are invaluable for understanding these complex rules.
- Data Encryption and Secure Payment Portals: Protecting sensitive financial and patient data requires robust security measures. Data encryption, secure networks, and compliant patient payment portals are essential to safeguard against cyber threats and maintain patient trust.
- Avoiding Billing Errors and Fraud Prevention: Proactive measures to prevent billing errors, such as thorough staff training, regular audits, and utilizing claims scrubbing technology, are vital. Furthermore, implementing strong internal controls helps prevent fraudulent activities, protecting both the practice’s finances and its reputation.
By prioritizing compliance and security within RCM, practices not only safeguard their financial assets but also build a foundation of trust with patients and payers.
Enhancing Operational Efficiency and Reducing Staff Burnout
Beyond financial health, the day-to-day operations of a medical practice significantly impact its overall success and the well-being of its staff. Streamlining workflows, optimizing resource allocation, and leveraging technology can dramatically improve efficiency and combat the pervasive issue of staff burnout.
The Central Nervous System: Practice Management Software (PMS)
Medical Practice Management Software (PMS) serves as the central nervous system for administrative operations. It’s a comprehensive platform designed to automate, streamline, and manage the non-clinical tasks essential to running a healthcare facility.
Core functionalities of PMS typically include:
- Appointment Scheduling: Intuitive scheduling tools allow staff to manage complex provider schedules, book appointments, handle cancellations, and send automated reminders, significantly reducing no-show rates.
- Patient Demographics and Registration: Centralizing patient information, including contact details, insurance data, and medical history summaries, ensures accuracy and quick access.
- Billing & Claims Management: As discussed in RCM, this includes charge capture, claims submission, payment posting, and denial management.
- Reporting & Analytics: Generating detailed reports on financial performance, patient flow, staff productivity, and other key metrics to inform decision-making.
- Patient Portal: Providing patients with secure online access to schedule appointments, view statements, communicate with the practice, and access health information.
Choosing the right PMS is a critical decision. Practices must consider their unique needs, specialty, size, and budget. While the benefits are substantial, practices often face challenges during adoption, including initial implementation costs, data migration from legacy systems, and staff training. However, the long-term gains in efficiency and reduced administrative burden typically outweigh these initial problems.
PMS vs. EHR: Understanding the Difference
It’s common to confuse Practice Management Software (PMS) with Electronic Health Records (EHR) systems, but they serve distinct, albeit complementary, purposes.
- PMS Focus: Primarily deals with the administrative and financial aspects of a practice. Think scheduling, billing, insurance, and reporting on operational metrics.
- EHR Focus: Concentrates on clinical data, including patient medical history, diagnoses, medications, treatment plans, lab results, and physician’s notes. Its main goal is to support clinical decision-making and patient care.
While some vendors offer integrated PMS/EHR solutions, many practices use separate systems. Integrating these systems can be challenging but offers significant benefits. When PMS and EHR communicate seamlessly, patient data flows effortlessly between administrative and clinical workflows, eliminating duplicate data entry and reducing errors. This integration leads to substantial time savings; practices using fully integrated software report weekly time savings of an average of four hours per clinician for documentation alone. For guidance on selecting such crucial systems, resources like the American Medical Association’s guide on choosing a practice management system can be very helpful.
Deployment Models and Modern Solutions
PMS solutions come in various deployment models, each with its own advantages and considerations:
- Cloud-Based (SaaS) PMS: This is the most prevalent model today. The software is hosted on remote servers and accessed via the internet.
- Pros: Lower upfront costs (subscription-based), accessible from anywhere with an internet connection, automatic updates and backups managed by the vendor, reduced IT overhead for the practice.
- Cons: Requires a reliable internet connection, data security relies on the vendor’s infrastructure, less customization flexibility.
- Client-Server PMS: The software is installed and run on local servers within the practice’s premises.
- Pros: Greater control over data and customization, potentially faster local network performance.
- Cons: High upfront costs for hardware and software licenses, requires dedicated IT staff for maintenance, updates, and backups, limited remote accessibility.
Here’s a quick comparison:
Feature Cloud-Based (SaaS) PMS Client-Server PMS Cost Subscription-based, lower upfront High upfront for hardware/software Accessibility Anywhere with internet access Primarily on-site, limited remote access Security Vendor-managed, requires trust Practice-managed, greater control Maintenance Vendor handles updates, backups Practice IT staff handles updates, backups Scalability Easily scalable up or down Requires hardware upgrades to scale IT Overhead Low High Modern PMS solutions often include mobile access, allowing providers and staff to manage tasks on the go, further boosting flexibility and efficiency. The shift to cloud-based solutions has also significantly reduced the IT overhead for many practices, allowing them to focus more on patient care and less on managing complex server infrastructure.
Strategic Sourcing and Partnerships in Medical Practice Management
Effective medical practice management extends beyond internal operations to encompass how a practice acquires the necessary resources to deliver care. Strategic sourcing of supplies and cultivation of strong vendor partnerships are crucial for cost control, maintaining quality of care, and ensuring operational continuity.
The Importance of a Streamlined Supply Chain
A well-managed supply chain is vital for several reasons:
- Inventory Management: Efficient inventory practices ensure that necessary medical supplies, pharmaceuticals, and office essentials are always available without excessive overstocking. This prevents shortages that could disrupt patient care and reduces waste from expired or unused products.
- Just-in-Time Ordering: Implementing just-in-time (JIT) ordering principles minimizes storage costs and ties up less capital in inventory, improving cash flow.
- Reducing Waste: Careful monitoring of supply usage and expiration dates helps reduce waste, which directly impacts the practice’s bottom line.
- Cost Analysis: Regularly analyzing the cost of supplies from different vendors helps identify opportunities for savings without compromising quality.
- Group Purchasing Organizations (GPOs): Many practices leverage GPOs to gain access to discounted pricing on supplies and equipment that they might not achieve individually. GPOs aggregate the purchasing power of multiple healthcare providers, negotiating better rates with manufacturers and distributors.
- Budgeting for Supplies: Accurate forecasting and budgeting for medical supplies are essential components of financial planning, preventing unexpected expenditures.
For practices looking to optimize their procurement processes and ensure a steady, cost-effective flow of essential items, exploring effective strategies for sourcing medical supplies is a wise investment of time. A robust supply chain is not just about cost savings; it’s about ensuring that our clinicians have the right tools at the right time to provide the best possible care.
Choosing the Right Vendors and Partners
Selecting the right vendors and partners is as important as managing internal operations. These relationships can significantly impact a practice’s efficiency, financial health, and reputation.
- Vendor Reputation and Reliability: Partnering with reputable vendors who have a track record of reliability, timely delivery, and quality products is paramount. Disruptions in supply can have direct consequences on patient care.
- Customer Support: Responsive and effective customer support from vendors is crucial, especially when issues arise with orders, equipment, or software.
- Pricing Transparency: Clear and transparent pricing, along with flexible payment terms, helps practices manage their budgets effectively.
- Technology Integration: For software vendors, seamless integration with existing PMS, EHR, and other healthcare IT systems is a key consideration to avoid data silos and workflow inefficiencies.
- Building Long-Term Relationships: Cultivating strong, long-term relationships with key vendors can lead to better pricing, preferential service, and collaborative problem-solving.
- Evaluating Service Level Agreements (SLAs): For critical services like IT support or specialized equipment maintenance, thoroughly reviewing and understanding SLAs ensures that the practice receives the agreed-upon level of service and support.
Strategic partnerships extend beyond physical supplies to encompass services like medical waste disposal, IT support, billing services, and even specialized clinical services. Each partnership should be evaluated based on its ability to improve the practice’s efficiency, reduce costs, and ultimately improve patient care.
Driving Growth by Elevating the Patient Experience
In today’s competitive healthcare landscape, patient experience is a powerful differentiator. Practices that prioritize and continuously improve how patients interact with their services are better positioned for growth, higher patient retention, and a stronger online reputation.

Modernizing Patient Interaction and Access
Technology has revolutionized how patients access and engage with healthcare. Practices that accept these digital tools can significantly improve the patient experience:
- Patient Portals: Secure online portals empower patients to schedule appointments, view lab results, access medical records, request prescription refills, and communicate with their care team. This self-service capability improves convenience and reduces administrative burden on staff.
- Online Appointment Scheduling: Offering 24/7 online scheduling caters to patient preferences and reduces phone call volume for front desk staff.
- Telehealth Integration: The rise of telehealth has made virtual consultations a standard offering. Integrating telehealth into practice workflows provides flexibility and accessibility for patients, especially for follow-ups or minor concerns.
- Automated Reminders: SMS and email reminders for appointments, follow-ups, and preventative screenings significantly reduce no-shows and improve patient adherence to care plans.
- Secure Messaging: Enabling secure, HIPAA-compliant messaging between patients and providers fosters better communication and allows for quick answers to non-urgent questions.
- Digital Intake Forms: Allowing patients to complete registration and medical history forms online before their appointment saves time during check-in and improves data accuracy.
By adopting these modern tools, practices demonstrate a commitment to patient convenience and engagement, which can lead to increased satisfaction and loyalty. Organizations like the American Medical Association provide resources and support for private practices navigating these advancements.
Expanding Service Lines to Meet Patient Demand
Strategic growth often involves identifying and responding to evolving patient needs and market trends. Expanding service lines can attract new patients, increase revenue, and provide more comprehensive care.
- Market Analysis: Regularly analyzing local demographics, competitor offerings, and patient feedback helps identify gaps in services or emerging demands.
- Identifying Growth Opportunities: This might involve adding services that complement existing offerings or addressing specific health concerns prevalent in the community.
- Adding Specialized Services: Examples include incorporating aesthetic procedures, offering comprehensive wellness programs focusing on nutrition and lifestyle, or introducing specialized treatments. For instance, practices are increasingly exploring offerings like specialized peptide weight loss treatments to address the growing demand for medically supervised weight management solutions.
- Staff Training for New Services: Successfully integrating new services requires investing in staff training and, if necessary, hiring personnel with specialized expertise. This ensures that the practice can deliver high-quality care in the new service area.
Careful planning, market research, and a commitment to quality are essential when expanding service lines. This approach not only drives growth but also improves the practice’s reputation as a comprehensive and forward-thinking healthcare provider.
Frequently Asked Questions about Medical Practice Management
How does effective practice management reduce staff burnout?
By automating repetitive tasks like appointment reminders, insurance verification, and basic patient inquiries, practice management software frees up staff to focus on higher-value activities and direct patient interaction. This reduction in administrative burden, coupled with streamlined workflows and improved job satisfaction, directly combats the causes of burnout. When staff feel more efficient and valued, their morale and retention significantly improve.
What is the first step in choosing a new Practice Management Software?
The first step is a thorough needs assessment. Before looking at any vendors, a practice must identify its biggest pain points, define its budget, and outline its key requirements. It’s crucial to involve stakeholders from administrative, clinical, and billing departments to ensure all needs and perspectives are considered. This comprehensive understanding will guide the selection process and help find a solution that truly fits the practice.
How does practice management impact patient retention?
Effective practice management directly improves the patient experience through conveniences like easy online scheduling, minimal wait times, clear communication, and transparent billing. A smooth, professional, and patient-centric administrative process builds trust and loyalty. When patients feel respected, informed, and efficiently cared for, they are more likely to return for future services and recommend the practice to others, thus boosting patient retention.
Conclusion
Medical practice management is the indispensable framework that underpins every successful healthcare organization. It’s a holistic approach that integrates financial stability, operational excellence, and an unwavering focus on the patient experience. By mastering Revenue Cycle Management, leveraging advanced Practice Management Software, strategically sourcing supplies, and embracing modern patient engagement tools, practices can not only steer the complexities of today’s healthcare landscape but also thrive within it.
The journey towards optimized practice management is one of continuous improvement, adaptation, and strategic investment. As healthcare evolves, so too must our management strategies. By prioritizing efficiency, compliance, and patient satisfaction, we ensure our practices remain resilient, profitable, and capable of delivering the highest quality of care, shaping the future of healthcare delivery for the better.


