The Hemorrhoid Banding Procedure: A Step-by-Step Guide

Hemorrhoids are a common and often uncomfortable condition that affects many adults. If you’ve experienced the itching, pain, or bleeding associated with them, you know how disruptive they can be to daily life. While many mild cases can be managed with home remedies, some persistent hemorrhoids require more definitive treatment.
This is where hemorrhoid banding, also known as rubber band ligation, comes in. It’s a widely used and effective non-surgical procedure designed to bring lasting relief.
What Are Hemorrhoids?
Hemorrhoids are swollen veins located in or around the anus and lower rectum. We categorize them into two main types:
- Internal Hemorrhoids: These form inside the rectum and are often painless, but can cause bleeding and sometimes prolapse (bulge out).
- External Hemorrhoids: These form under the skin around the anus and can be painful, itchy, and may bleed.

When internal hemorrhoids become problematic—causing persistent bleeding, discomfort, or prolapse—banding offers a proven solution.
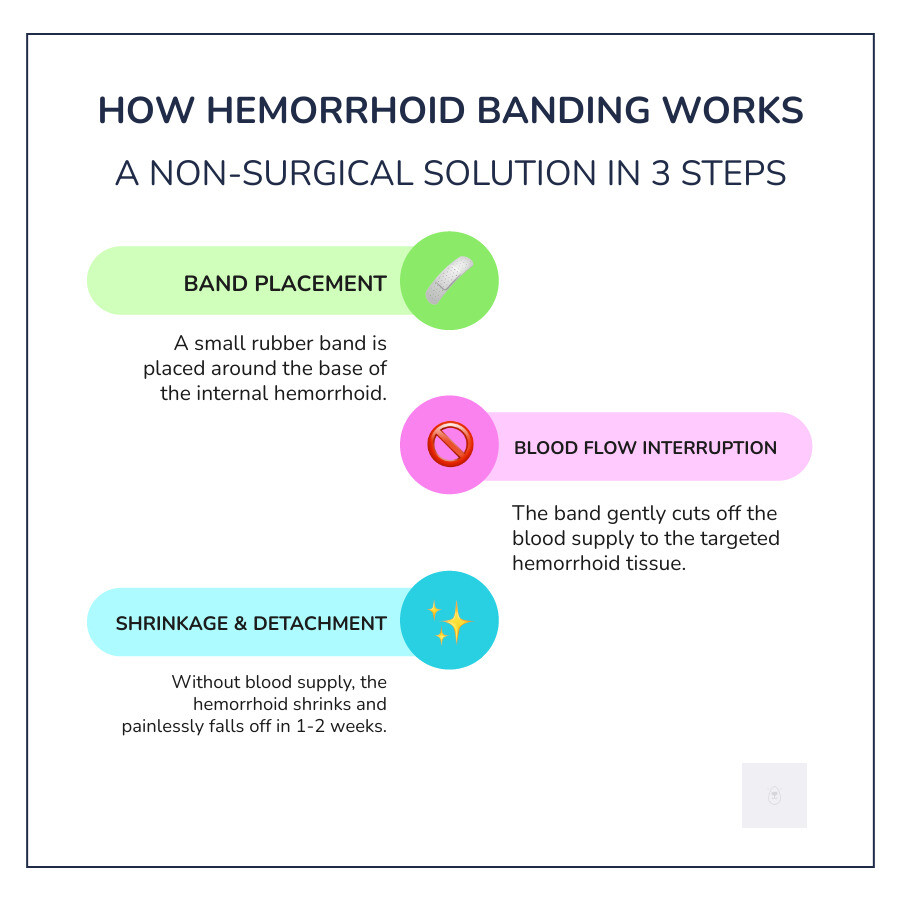
How Does Hemorrhoid Banding Work?
Hemorrhoid banding is a minimally invasive procedure that targets the problematic internal hemorrhoids. It involves placing a small rubber band around the base of the hemorrhoid. This band gently cuts off the blood supply to the tissue. Without blood flow, the hemorrhoid will painlessly shrink and fall off within one to two weeks, often during a bowel movement. A small scar forms in its place, which helps prevent future recurrence in that area.
Understanding the various grades of internal hemorrhoids and how banding addresses them is key. For those seeking specialized care and information on gastroenterology hemorrhoid banding, consulting with experts is crucial for personalized treatment plans.
In this comprehensive guide, we will explore everything you need to know about hemorrhoid banding. We’ll cover who is a good candidate, what to expect during the procedure, the recovery process, and how it compares to other treatment options. Our goal is to provide you with clear, reliable information to help you understand this effective solution.
Hemorrhoid banding is a straightforward, often quick procedure that can be a game-changer for individuals suffering from persistent internal hemorrhoids. It’s typically performed as an outpatient procedure, meaning you won’t need an overnight hospital stay. In many cases, doctors can even perform it right in their office, making it a convenient option for many patients. The entire process typically takes only a few minutes, although it may extend if multiple hemorrhoids are being addressed over several sessions.

Who is a Candidate for Hemorrhoid Banding?
While hemorrhoid banding is highly effective, it’s not suitable for everyone or every type of hemorrhoid. The procedure is primarily designed for internal hemorrhoids, which are located above the dentate line in the anal canal, where there are fewer pain-sensing nerves.
We typically recommend banding for patients with:
- Grade I internal hemorrhoids: These bleed but do not prolapse.
- Grade II internal hemorrhoids: These prolapse during defecation but spontaneously reduce.
- Grade III internal hemorrhoids: These prolapse during defecation and require manual reduction.
Banding is often considered when conservative treatments, such as a high-fiber diet, increased fluid intake, cold compresses, sitz baths, and topical creams, have failed to provide lasting relief from symptoms like bleeding, itching, pain, or discomfort. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), rubber band ligation is a common and effective treatment for internal hemorrhoids that don’t respond to home treatments.
However, there are certain situations where banding might not be appropriate. These contraindications include:
- Grade IV hemorrhoids: These are permanently prolapsed and cannot be manually reduced. Surgery is often a more suitable option for these advanced cases.
- External hemorrhoids: These are located below the dentate line, an area rich in pain-sensing nerves, making direct banding too painful and ineffective. We will discuss this further in the FAQ section.
- Anal fissures or active infections: These conditions need to be treated first before considering banding.
- Patients on certain medications: Individuals taking blood thinners or with compromised immune systems may also not be ideal candidates due to increased risks of bleeding or infection. Always disclose all medications and supplements to your doctor.
- Crohn’s disease: Patients with Crohn’s disease may also have contraindications due to increased risk of complications.
Even if you experience symptoms commonly associated with external hemorrhoids, internal hemorrhoid banding can sometimes provide relief. Around 90% of patients with external hemorrhoid symptoms find relief with internal hemorrhoid banding, as treating the internal component can reduce overall pressure and swelling.
How to Prepare for the Procedure
Preparing for hemorrhoid banding is generally less involved than for surgical procedures, but it’s still crucial to follow your doctor’s specific instructions.
- Consultation is key: Before anything else, you’ll have a thorough consultation with your doctor. This is your opportunity to discuss your medical history, current symptoms, and any concerns you may have. Your doctor will examine you to determine if banding is the right treatment for you.
- Medication disclosure: We cannot stress enough the importance of informing your doctor about all medications, over-the-counter drugs, vitamins, and herbal supplements you are taking. This is especially critical if you are on blood thinners (like aspirin, warfarin, or NSAIDs such as ibuprofen or naproxen), as these can increase the risk of bleeding during or after the procedure. Your doctor may advise you to stop taking these medications temporarily.
- Fasting and sedation: Many modern banding techniques, particularly those using advanced suction ligators, do not require sedation. In these cases, you typically won’t need to fast. However, if your doctor plans to use sedation, you will likely need to avoid eating or drinking for several hours before the procedure. Always clarify these instructions with your healthcare provider.
- Bowel preparation: For most office-based banding procedures, extensive bowel preparation (like a full colonoscopy prep) is rarely needed. You may be asked to use a simple enema beforehand, but this is not always necessary. Your doctor will provide precise instructions if any bowel prep is required.
- Arranging transportation: If any form of sedation is used, or if you anticipate significant discomfort, it’s advisable to arrange for someone to drive you home after the procedure. Having someone stay with you for the first day or two can also be beneficial, especially in helping to avoid any straining that could complicate recovery.
What Happens During the Banding Process?
The actual hemorrhoid banding procedure is relatively quick and efficient. Here’s a general overview of what you can expect:
- Patient Positioning: You’ll typically be asked to lie on your side or in a position that allows easy access to the anal area, similar to a standard rectal exam.
- Anoscope Insertion: Your doctor will gently insert a small, lighted tube called an anoscope into the anal canal. This instrument enables clear visualization of internal hemorrhoids.
- Ligator Tool: A specialized tool called a ligator is then passed through the anoscope. Depending on the technique, this ligator might use small forceps or gentle suction to grasp the hemorrhoid.
- Band Placement: Once the hemorrhoid tissue is securely drawn into the ligator, a small rubber band is released and placed around the base of the hemorrhoid. This band constricts the blood supply.
- Sensation of Fullness: You might feel a mild sensation of pressure or fullness in your rectum immediately after the band is applied. This is usually not painful, as the band is placed in an area with few pain-sensing nerves.
- Procedure Duration: The placement of each band takes only a matter of seconds to a few minutes. For multiple hemorrhoids, your doctor may treat only one or two at a time during a single visit to minimize discomfort and reduce the risk of complications. Subsequent visits, typically spaced a few weeks apart, would then be scheduled to band other hemorrhoids.
After the band is in place, the instruments are carefully removed. You’ll then be given post-procedure instructions and can usually go home shortly after.
Comparing Hemorrhoid Banding Techniques and Alternatives
Hemorrhoid banding isn’t a monolithic procedure; different techniques exist, and it’s also one of several options for hemorrhoid treatment. Understanding these variations and how banding compares to other therapies can help you make an informed decision.
We cannot create a table here, but we can compare the techniques and alternatives in detail.
Traditional vs. Modern Banding Methods
The core principle of rubber band ligation—cutting off the blood supply—remains the same across techniques, but the tools and approach have evolved.
- Traditional Rubber Band Ligation: This method typically involves using a metal clamp or forceps to grasp the hemorrhoid, followed by the application of a rubber band. While effective, it can be associated with more discomfort. Studies indicate that pain occurs in about 25% to 50% of patients after traditional rubber band ligation, and recovery can take up to three days. The procedure itself might take 5 to 10 minutes per hemorrhoid.
- Endoscopic Banding: This technique uses an endoscope, a flexible tube with a camera, to visualize and band hemorrhoids. While it offers excellent visualization, it often requires fasting, bowel preparation, and sedation, making it a more involved procedure than office-based banding.
- Modern Suction Ligation (e.g., CRH O’Regan System): This represents a significant advancement in banding technology. Instead of metal clamps, devices like the CRH O’Regan ligator use gentle suction to draw the hemorrhoid tissue into the device before the band is released. This suction-based approach is designed to be less painful, as it avoids pinching the tissue with forceps. The CRH O’Regan System is particularly notable for its efficiency and patient comfort. It has been proven to be 99% effective, with fewer than 1% of patients experiencing significant pain or other complications. The procedure itself is incredibly fast, often taking less than a minute per hemorrhoid, and typically requires no preparation or sedation. This allows patients to return to their normal activities, including work, almost immediately.
How Banding Compares to Surgical Removal
For many patients, banding offers a compelling alternative to more invasive surgical options.
- Hemorrhoidectomy: This is a surgical procedure that involves the removal of hemorrhoids. During a hemorrhoidectomy, the surgeon makes incisions around the hemorrhoid and ties off the swollen vein before removing the tissue. This is a highly effective treatment, but it is considerably more invasive. It typically requires general anesthesia, a hospital stay, and a significantly longer and often more painful recovery period, which can extend over a month. The risk of complications is also higher compared to banding. Hemorrhoidectomy is generally reserved for very large, symptomatic Grade IV hemorrhoids or cases where other less invasive treatments have failed.
- Coagulation Therapy (Infrared Photocoagulation): This method uses infrared light to create scar tissue that cuts off the blood supply to the hemorrhoid. It’s less invasive than banding but often less effective for larger hemorrhoids and may require more treatment sessions.
- Sclerotherapy: Involves injecting a chemical solution into the hemorrhoid to shrink it. It’s generally well-tolerated but may have a higher recurrence rate than banding.
- Cryosurgery: Freezes the hemorrhoid with a cryoprobe, causing it to fall off. Patients often experience pain, and there’s a risk of infection.
- Stapling (Procedure for Prolapse and Hemorrhoids – PPH): This procedure uses a stapling device to remove a ring of tissue above the hemorrhoids, lifting and shrinking them. While less painful than a traditional hemorrhoidectomy, it still involves general anesthesia and carries a risk of complications and recurrence.
Hemorrhoid banding, by contrast, is not considered a surgical procedure because it does not involve incisions. It is widely regarded as the most effective non-surgical treatment for internal hemorrhoids. While highly successful, it’s important to understand that up to 1 out of 10 people may still need surgery after hemorrhoid banding if their symptoms persist or recur.
GastroDox’s Specialized Hemorrhoid Banding: Recovery and Effectiveness
After undergoing hemorrhoid banding, most patients are pleasantly surprised by the relatively quick and manageable recovery process. The goal of this treatment is not only to eliminate existing hemorrhoids but also to provide lasting relief, allowing you to return to your daily life with minimal disruption.

The Recovery Process After GastroDox’s Specialized Hemorrhoid Banding
The recovery experience can vary slightly depending on the individual and the specific banding technique used, but here’s a general overview of what you can expect:
- Timeline: The banded hemorrhoid typically dries up and falls off within one to two weeks after the procedure. You may not even notice it, as it often occurs during a bowel movement. The rubber band itself is very small and may be seen in the toilet. The tissue where the hemorrhoid was will then form a small scar as it heals over the next few days.
- Return to Work and Activities: One of the significant advantages of modern banding techniques, such as the CRH O’Regan System, is the minimal downtime. Many patients can return to work or resume most normal activities immediately after the procedure, provided their job doesn’t involve strenuous physical activity. For more traditional banding methods, you might need a day or two of rest. We generally advise avoiding heavy lifting and vigorous exercise for about two to three weeks to prevent straining.
- Expected Sensations: It’s common to experience a sensation of fullness or a dull ache in the rectum for the first 24 to 48 hours. This is usually mild and manageable with over-the-counter pain relievers, such as acetaminophen or ibuprofen. Sharp or severe pain is uncommon, especially with modern techniques, and should be reported to your doctor.
- Minor Bleeding: A small amount of bleeding is normal, particularly when the banded hemorrhoid finally falls off. This might appear as a few drops of blood on toilet paper or in the toilet bowl. However, persistent or excessive bleeding (more than a few tablespoons) is not normal and warrants immediate medical attention.
- Aftercare Tips: To promote healing and comfort, we recommend several aftercare practices:
- Sitz Baths: Soaking in a warm sitz bath for 15-20 minutes, two to three times a day, and after bowel movements, can help soothe the area and keep it clean.
- High-Fiber Diet and Fluids: Maintaining a diet rich in fiber (aim for 14 grams per 1,000 calories) and drinking plenty of water is crucial. This helps soften stools, preventing constipation and straining, which can irritate the healing area and contribute to the development of new hemorrhoids.
- Stool Softeners: Your doctor may recommend over-the-counter stool softeners to help ensure smooth and effortless bowel movements.
- Avoid Straining: This is paramount. Do not strain during bowel movements. A small step stool can help optimize your position.
- Cold Packs: Applying a cold pack wrapped in a cloth to the area for 10-20 minutes at a time can help reduce swelling and discomfort.
- Adequate Rest: Listen to your body and get sufficient rest.
Monitoring for and promptly reporting any concerning symptoms to your doctor is a key best practice for a smooth recovery.
Understanding the Efficacy of GastroDox’s Specialized Hemorrhoid Banding
Hemorrhoid banding boasts impressive success rates, making it a preferred non-surgical option for many.
- Effectiveness Statistics: In general, the success rate of hemorrhoid banding ranges from 70% to 97%. This means that about 8 out of 10 people find significant relief from their symptoms. With advanced systems like the CRH O’Regan System, effectiveness is even higher, proven to be as high as 99%. This high success rate positions banding as a highly reliable treatment.
- Recurrence Rate: While no hemorrhoid treatment guarantees permanent eradication, banding significantly reduces the likelihood of recurrence. With modern techniques, such as the CRH O’Regan System, fewer than 5% of patients experience a recurrence within two years. This long-term effectiveness is a major benefit compared to some other treatments.
- Cost-Effectiveness: Hemorrhoid banding is also a cost-effective solution. A 2019 study indicated that the average cost of hemorrhoid banding is around $723, which is considerably less than the cost of surgical alternatives.
The expertise in performing these procedures, particularly specialized approaches, minimizes risks and improves outcomes for patients.
Frequently Asked Questions about Hemorrhoid Ligation
We understand that you likely have many questions about hemorrhoid banding. Here, we address some of the most common concerns to provide further clarity.
Is Hemorrhoid Banding Painful?
This is one of the most frequently asked questions, and for good reason. The good news is that the banding procedure itself is generally painless. This is because the rubber band is strategically placed above the dentate line in the anal canal, an area with a very low density of pain-sensing nerves. You may experience a sensation of pressure or fullness, but typically not sharp pain, during the actual banding.
However, post-procedure discomfort can vary depending on the technique used. Traditional banding methods, which often use metal clamps, can sometimes lead to more post-procedure pain, affecting 25% to 50% of patients. Modern suction ligation systems, like the CRH O’Regan System, are designed to minimize this discomfort. Less than 1% of patients experience significant pain or other complications with these advanced methods, reporting only a dull ache or feeling of fullness that is easily managed with over-the-counter pain relief.
Can External Hemorrhoids Be Treated with Banding?
No, external hemorrhoids cannot be directly treated with banding. External hemorrhoids are located below the dentate line, where there are abundant pain-sensing nerves. Attempting to band an external hemorrhoid would be extremely painful and is not an effective treatment method.
Hemorrhoid banding is exclusively used for internal hemorrhoids. However, it’s worth noting that internal hemorrhoids, especially prolapsed ones, can sometimes contribute to the symptoms of external hemorrhoids by causing swelling and pressure. In such cases, treating the internal hemorrhoids with banding can indirectly alleviate symptoms associated with the external ones. In fact, around 90% of patients with external hemorrhoid symptoms find relief with internal hemorrhoid banding, as the reduction in internal pressure and swelling can significantly improve overall comfort.
What Should I Expect Regarding Bowel Movements After the Procedure?
After hemorrhoid banding, it’s common to feel a sensation of needing to defecate, even if your bowels are empty. This is due to the presence of the band and the slight swelling in the area. This feeling usually subsides within one to two days.
The most important thing to remember regarding bowel movements after the procedure is to avoid straining. Straining can put undue pressure on the healing area, potentially causing pain or prematurely dislodging the band. To facilitate soft, easy bowel movements, we strongly recommend:
- Using stool softeners: Your doctor may prescribe or recommend an over-the-counter stool softener.
- Maintaining a high-fiber diet: Incorporate plenty of fruits, vegetables, whole grains, and beans into your diet. The recommended intake is about 14 grams of fiber per 1,000 calories consumed.
- Drinking plenty of fluids: Staying well-hydrated helps keep stools soft.
When the banded hemorrhoid falls off (typically within two to four days, but sometimes up to two weeks), you might notice a small amount of blood in your stool or on the toilet paper. This is expected. However, if you experience excessive bleeding (more than a few tablespoons) or persistent bleeding that doesn’t stop after two or three days, you should contact your doctor immediately.
Conclusion: Is Hemorrhoid Banding Right for You?
Hemorrhoid banding offers a highly effective, minimally invasive, and generally well-tolerated solution for problematic internal hemorrhoids. Throughout this guide, we’ve explored its core principles, the step-by-step process, comparisons with other treatments, and what to expect during recovery.
To recap, the key benefits of hemorrhoid banding include:
- Minimally Invasive: This is an office-based procedure that eliminates the need for surgery, general anesthesia, or hospitalization.
- High Success Rate: With success rates ranging from 70% to 99% depending on the technique, it provides lasting relief for a vast majority of patients.
- Quick Recovery: Most patients experience minimal downtime, often returning to work and their daily activities immediately or within one to two days.
- Low Pain: Modern banding techniques are designed to be painless during the procedure, with only mild, manageable discomfort during recovery.
- Targeted Treatment: It effectively addresses symptomatic internal hemorrhoids that haven’t responded to home remedies.
If you are experiencing persistent symptoms such as bleeding, itching, pain, or prolapse from internal hemorrhoids, we encourage you to consult with a board-certified gastroenterologist. They can provide a personalized assessment, discuss whether hemorrhoid banding is the right treatment option for your specific situation, and guide you through the process. Don’t let hemorrhoids dictate your comfort and quality of life—effective solutions are available.
